By Palmer R. Cook, OD
Every day, eyecare practitioners deal with patients of all ages, and those dealings are intuitively or intentionally, guided by each patient’s age. For the most part, those aged 50 and beyond belong to the GI Generation (born 1901 to 1926), the Mature/Silent Generation (born 1927 to 1945) or the Baby Boomer Generation (born 1946 to 1964). The most recognized ocular commonality that members of these generations share is presbyopia. Thankfully, most of them are no longer “presbyopes in denial,” a phenomenon of which all optometrists, ophthalmologists and opticians are acutely aware. However, there are other time-related ocular changes that often affect how we deal with their eye and vision needs.
NORMAL, HEALTHY EYES OF THE 50+ PATIENT
A gradual reduction in the diameter of the pupil occurs with time. This alone may require modifying exam and treatment protocols for patients halfway and more toward their first triple-digit birthday. These patients experience glare issues and lengthened glare recovery times to the point of reducing visual performance. Anatomical changes within the crystalline lens may cause a refractive shift toward more hyperopia or less myopia. The lids as well as the conjunctiva become thinner and less elastic, and the lacrimal glands tend to be less productive. The reflectance of the corneal epithelium is reduced giving a more “dull” appearance to the eye. A yellowing of the sclera also tends to occur. The crystalline lens becomes less transparent, causing increased scattering of light.
Presbyopia is the loss of the ability of the eye to change focus sufficiently to meet normal demands on the visual system. Presbyopia is as inevitable as taxes and similarly annoying when you begin to experience it. Its onset becomes noticeable between ages 40 to 45 for most. Our eyes are gifted with the ability to change focus between distance and near objects, but the gift is only a loan, and for most of us the loan runs out in our 40s.
Presbyopia results from a gradual thickening of the lens of the eye. This ultimately reduces and finally eliminates the ability of the lens to change shape. When the lens assumes a steeper curvature it has more plus power, and with less curvature it has less plus power.
The lens, although transparent, bears similarity to the “stone” found in the center of every peach. Its nucleus is somewhat like the bitter seed revealed when the stone is split open. The hard, protective covering of that bitter seed could represent the layers that are gradually formed as we age. The seed could represent the center or nucleus of the lens, which was the lens of the eye at birth.
An elastic capsule surrounds the lens. When the ciliary muscle contracts, tension is reduced on the threads (i.e., the zonules of Zinn) that hold the lens in place. As the zonules relax, the elastic capsule squeezes the lens into a more steeply curved shape, and the eye’s optical power is increased. This process is called accommodation, and it allows us to focus on near objects.
An early symptom of presbyopia is a need to hold reading material further from the eyes. This is often closely followed by a need for brighter light for near vision. The eye’s natural defense against presbyopia is the decrease in pupil size that occurs as we age. With smaller pupils, the size of the blur circles that make up the retinal image are reduced, sharpening the image, and this partially compensates for lost accommodation.
Lenticular changes also account for continued loss of whatever accommodative ability may have remained as the half-century mark was met. Although, in the absence of pathological changes, the retinal function at the macula tends to remain intact, but dark adaptation is reduced. These are among the “normal” eye and vision changes that occur as we age, and we should take them into account as part of providing the best in vision care.
PATHOLOGICAL CHANGES
Ocular pathology such as cataract, glaucoma, macular degeneration, fluctuating refractive error, optic atrophy, ptosis (drooping eyelids), entropion (a painful in-turning of the lids—most often the lower lid) and many less frequent eye-related conditions are found commonly beyond age 50. Generally, pathological changes affecting the eye and vision require medical or surgical treatment, yet often eyewear can be designed to lessen the impact or slow the onset of some of these conditions.
| Lens Material | Index | Reflectance | T% | Gh% |
| Standard Plastic | 1.498 | 3.97% | 92.2 | 100% |
| Crown Glass | 1.525 | 4.32% | 91.5 | 117% |
| Trivex P. | 1.53 | 4.39% | 91.4 | 121% |
| Mid-index Plastic | 1.56 | 4.79% | 90.7 | 143% |
| Polycarb. P | 1.59 | 5.19% | 89.9 | 167% |
| Mid-index Glass | 1.60 | 5.33% | 89.6 | 176% |
| Mid-index Plastic | 1.60 | 5.33% | 89.6 | 176% |
| High-index Plastic | 1.66 | 6.16% | 88.1 | 230% |
| High-index Glass | 1.706 | 6.81% | 86.8 | 278% |
| Thin & Lite | 1.74 | 7.29% | 85.4 | 315% |
| Very High-index Glass | 1.80 | 8.16% | 84.3 | 387% |
| Very High-index Glass | 1.893 | 9.53% | 81.8 | 512% |
TABLE 1. Lens transmittance (4th column from the left) is reduced by reflectance at each lens surface. The percent reflected at each surface (3rd column) increases as the index of the material increases. Materials represented here are non-tinted, non-AR, and the percentages shown do not include light lost by absorption or scatter. For purposes of comparison the brightness of "ghost" or secondary images (far right column) formed by the lowest index material, standard plastic, is assigned a value of 100%, and the brightness of those images for other materials is shown in comparative percentages (e.g., Glass with a 1.893 index would have secondary images more than 5 times as bright as standard plastic – actually 412% greater).
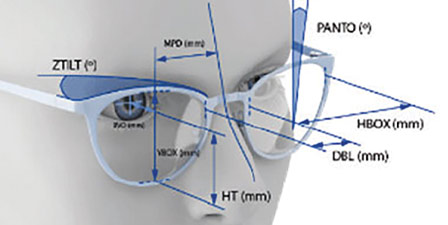
Figure 1A
Internally reflected light causes a veiling of the retinal image. The internally reflected ray path is the same one that causes ghost images of headlights and other bright light sources when driving after dark.
Figure 1B
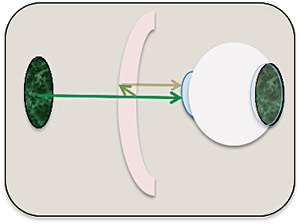
A light tint selectively reduces veiling glare because the primary ray bundle passes through the tint only once, while the internally reflected light passes through the lens three times.
Figure 1C
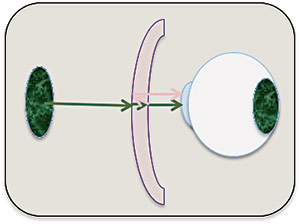
When the lens is made anti-reflective and a light tint is included, the veiling caused by internal lens reflections is reduced further.
Light is the form of energy that makes vision possible. A reduction in pupil diameter decreases the amount of light reaching the retina. Older eyes need more light, and this is not only due to decreased pupil size. Light absorption and scatter resulting from changes in the cornea and lens, and reduced retinal sensitivity are also causative factors. This makes poorly illuminated stairways more hazardous and the same goes for night driving or negotiating unfamiliar, possibly cluttered, areas in the home and elsewhere.
It’s important to remember that the transmittance of lens materials decreases as index increases (Table 1). This is primarily due to increased reflectance of the lens materials. This effect is significantly reduced when the lenses are made anti-reflective. Light tints tend to improve the quality of the retinal image because they decrease veiling resulting from increased lens reflections (Fig. 1A and 1B). Many patients insist a light tint they formerly found helpful be continued with new eyewear.
A problem can arise with these tints because the tints fade over time, and the new lenses will absorb more light than the previous lenses. This reduced transmittance can lead to problems with night driving for the now older and less sensitive retinas. Even if the patient has not had a tint previously, light scatter may lead patients to request for some tint or a photochromic material. Use caution when adding a tint of any kind to higher index lenses, particularly for patients over 50.
The brightness of the secondary or “ghost” images shown in Table 1 is important for aging patients because their retinas require more light to form a usable primary retinal image, but the secondary image formed, which degrades the primary retinal image, is made up of light lost by internal lens reflectance. When AR lenses are prescribed, the secondary images are diminished by wave cancellation or destructive interference, while constructive interference increases the amplitude of the light making up the primary ray bundle (Fig. 1B and 1C). The result is a sharper, brighter retinal image for your patient.
Although some laboratories are reluctant to combine a light tint with AR because it is hard to control the lightening of the tint that occurs during the AR processing, the combination of a light tint will improve optical performance. If you are providing photochromic lenses with AR, using a photochromic that has some residual tint when fully lightened will also tend to improve the performance of the AR.
ON THE BRIGHTER SIDE
Night myopia is an apparent shift toward more myopia (or less hyperopia) caused by excessive accommodative efforts, dilated pupils and the natural chromatic aberration of the eye. Because of this, astute docs may shift the prescription for sun lenses for younger patients toward slightly less plus or more minus. For 50 and beyond patients, the lack of accommodation and less active pupils usually make this adjustment for prescription sun lenses unnecessary.
DRY EYES
Dry eye complaints are more common among patients over 50. In addition to medical treatment, selecting eyewear with wide temples and/or some facial wrap to limit airflow may help. Patients should also be made aware that long hours on the computer and long distance driving tends to reduce blink rates and can make dry eye symptoms worse. In cold weather, using a humidifier in your car and keeping your ventilation system on recirculate most of the time can also help. In the case of severe dry eye, moisture chamber glasses can be considered.
GLARE AND FLARE
Glare is a phenomenon in which extraneous light interferes with clear, comfortable vision. The light that causes glare is often excessively bright, reflected and/or misdirected. Glare degrades the visual experience and can cause discomfort or pain. While eyes of all ages are subject to glare, older eyes are especially prone to flare, which is sometimes referred to as veiling glare. Flare degrades the retinal image, and it results from light scattered within the eye.
Often those 50 and beyond have discovered the significant relief they get from blocking overhead light sources, and they begin wearing ball caps. However, they universally wear them with the bill forward, unlike the 25 and younger folks who tend to wear them the other way around.
Figure 2


In the left photo, paper on the dash is creating a veiling glare. The right picture was taken with a tan polarizing lens over the camera lens. The light reflected from the dash to the windshield strikes at about Brewster’s angle, which polarizes the reflection allowing it to be blocked by the polarizing lens as shown in the right picture. Windshields are tilted at this angle to improve aerodynamics and increase gas mileage. Ideally, dashboards should be flat black and dust-free to reduce this reflectance problem. Vinyl and leather treatments that make the dash more reflective should be avoided. The tan tint further reduces blue light and intraocular light scatter.
Glare recovery time is the length of time needed for previously visible objects to reappear after exposure to glare. Glare recovery time is dependent on the intensity and duration of the glare. For eyes of 50 and beyond, glare recovery time increases significantly. Oncoming headlights at night are an example of glare that is often exacerbated in eyes subject to internal light scatter and prolonged glare recovery time.
Using a dark gradient that “fast-fades” to little or no tint for straight ahead vision can be especially helpful for these older patients. With such a gradient the wearer can anticipate and block glare by dropping his chin to look through the tint and raising his chin to view through the part of the lens with little or no tint when the glare source is gone. This sidesteps the issue of glare recovery in many situations.
Not all glare is caused by reflected light, however when light is reflected at Brewster’s angle it is polarized and can be selectively blocked using lenses which are polarized at right angles to the polarization of the reflected light. Polarizing lenses are highly effective in reducing glare caused by light reflected from horizontal surfaces, and they have absorptive tints to reduce overall brightness. Light reflecting from the dash to the windshield and then to the driver’s eyes is often a less intense form of glare but it is tiring and sometime debilitating to the point of causing accidents. Using polarizing lenses for daylight driving effectively eliminates this source of glare (Fig. 2). The selective glare elimination property of polarizing lenses uniquely qualifies them as the best choice for protection against reflected glare even though they will not selectively reduce the veiling glare caused by filmed windshields or light scattered within the eye.
Glare from a car’s windshield can occur when a heavy filming suddenly glows as you turn to face bright sunlight. It can also result from filming on the inside of the window caused by smoking and condensation. The eyes of patients 50 and beyond are more likely to have ocular changes that make them more susceptible to glare problems of all types.
HIGHER ADDS
For most patients, prescribers assume a 40 cm (16 inch) reading distance. As presbyopia advances, the add power is increased, creating a need for an intermediate power for some tasks. It is not uncommon for stronger adds to be prescribed when the distance acuity can no longer be corrected to 20/20. Using a +3.00 add allows the patient to have a clear focus at about 33 cm, and this effectively makes print larger, but it also requires more convergence and more decentration of the adds.
When adds were provided with segs that had widths of 28 mm, 35 mm and wider usable areas, near PDs were taken with the eyes converging in the straight ahead position giving “too wide” results, but that caused few problems. For patients with binocular vision, adds that are misplaced lose 2 mm of usable width for every 1 mm error in the near PD.
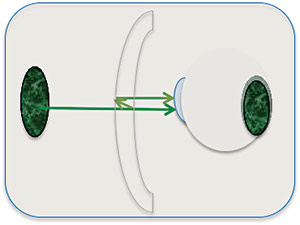
Figure 3
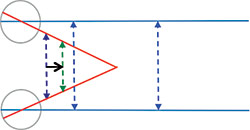
Seen from above, the parallel solid blue lines represent the parallel lines-of-sight viewing an object on the horizon. The red lines represent the lines-of-sight converging to view a near object. It is clear that as the vertex distance changes (purple to green arrow), the separation of the points at which the lines of sight intersect the lens will lessen.
Figure 3A
Viewed from the side, it is apparent that the vertex distance in this example, as in the case of most patients, is shorter for distance viewing (shown by the green arrow) and greater when the patient looks down near viewing.
If a PAL is used, contact your lab to find the inset of the Near Reference points (NRPs) for the design of choice and mark those points on the lenses at the height of the NRPs with a lens marking pen. After fully adjusting the frame, ask the patient to look at a target held at the focal distance of the add (e.g., for a +3.00 add the distance would be 33 cm). Then cover one of the patient’s eyes and ask him to raise his chin and turn his head until he is looking through the mark. Next, being careful that the patient does not move his head and without moving the target, move the cover to the patient’s other eye and ask if he is looking through the dot on that lens. For distances closer than 40 cm, it is likely that the patient will report that the dot on the second lens is outward toward his ear, indicating that the separation of the NRPs for that design is too wide. You may be able to correct this by increasing the pantoscopic tilt (Fig. 3 and 3A). If that proves to be impractical, consider recommending reading glasses for prolonged near tasks.
As print is moved closer, the angle through which the eyes must move to traverse the line without head movement becomes greater. Therefore, patients will find their field of binocular central vision is narrowed, which may be very annoying. This effect is due to relative distance magnification and optical magnification as well as a too-small reading area in the lens and a too-wide or too-narrow separation of the NRPs.
NOSE POINTING
At 50 and beyond, many people experience problems of arthritis and other maladies that can restrict head movement, and they often experience other physical restrictions such as difficulty walking or holding reading material. We all have counseled PAL wearers to become “nose pointers,” to help them avoid the “optically disadvantaged” areas of their lenses. Yet the constant head movements required for reading with a PAL can be problematic for some seniors.
For many of these patients, especially those using walkers, a low-set lined-bifocal supplemented by prescription reading glasses may be a good solution.
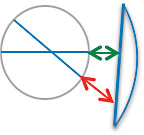
Figure 4

Ptosis crutches slide below the roof of the orbit, supporting lids that droop and tucking excess lid tissue out of the way in cases of blepharochalasis. The frame and the crutch(es) should be carefully adjusted so that the upper and lower lids come into contact when the patient blinks, otherwise the corneal epithelium will dry and erode.
Ptosis (pronounced toe-sis) is a downward displacement or sagging of the upper lid. It can be bilateral or unilateral, mild or marked (blocking the pupil), and it can result from a variety of problems including neurological, congenital and even a vitamin deficiency. Blepharochalasis (blef-row-shall-a-sis) is an increase in the skin of the upper eyelid due to a loss of elasticity. In advanced blepharochalasis, the lid tissue may droop over the edge of the lid obscuring vision. Both ptosis and blepharochalasis require a careful diagnosis, and the treatment may be either medical or surgical. When either condition has stabilized, the lid(s) may continue to interfere with vision. If the patient is unwilling or unable to have surgery as in the case of some older patients, a ptosis crutch is sometimes used to give temporary or prolonged relief (Fig. 4).
Figure 5

Entropion crutches keep the lower edge of the tarsal plate in the lower lid from flipping outward so the plate is in a more or less horizontal position. Often it can be seen jutting forward under the skin of the lower lid. The frame should be adjusted so that it will stay in place comfortably without sliding downward. The entropion crutch should then be adjusted so that there is light pressure on the edge of the plate. This will cause it to flip inward, positioning the plate so that it is more or less parallel to the surface of the sclera and eliminating the entropion. When the lid is not inverted, the pad of the entropion crutch should still exert light contact with the lid to prevent reoccurrence of the inversion.
Another condition more commonly found in older patients is entropion. Entropion is an inversion of the lower lid usually due to scarring of the lining of the lid (i.e., palpebral conjunctiva) or less commonly, spasm of the orbicularis muscle. It causes the eyelashes to abrade the cornea, and it is painful. Surgery is usually recommended for entropion, however if surgery is not an option, an entropion crutch can give substantial relief (Fig. 5). Entropion crutches are not as effective with spastic entropion.
EYEWEAR WEIGHT
Heavy glasses slide down more, and the pads can cause indentations on the nose. New eyewear pads should not bear on such indentations. Also a Trivex-type material, with its excellent optical properties and weight lighter than any other ophthalmic material over a wide range of prescriptions can be helpful.
EYEWEAR HYGIENE
Dirty lenses interfere with vision, and buildup on nosepads can cause skin irritation. Suggest a weekly soak in water with a little Dawn dishwashing detergent. Dawn has a pH nearer neutral than most detergents, and it is unlikely to affect lens coatings or frame finishes. Everything changes as time passes, and our visual systems are no exception. Your 50 and beyond patients may need a little special attention, but that’s just part of providing excellent eyecare. ■
Contributing editor Palmer R. Cook, OD, is an optometric educator and optical dispensing expert.
The ptosis and entropion crutches in this article were fabricated by Arthur E. Brown, of Northhampton, Pa., qualityoptician.com