Photography by Bleacher + Everard
BY BARRY SANTINI
PART ONE OF A TWO-PART SERIES
In our day-to-day roles, eyecare professionals often give little additional thought about how a disparate prescription might impact that patient’s comfortable binocular vision (BV). Significant monocular Rx changes—such as those introduced by a maturing cataract—might occasionally get our attention. But in general, most ECPs don’t typically think: “What should I do to ensure optimal binocular vision with this prescription?” Why? One reason is most people “appear” to adapt to changes in a newly Rxed pair of glasses. Another reason is the old advice that’s continually whispering in our ear: “Don’t fix what ain’t broken.” What’s common to both of these explanations is unfortunate: They rely on an “absence of complaint” as a surrogate for more hard knowledge about the exact state of that person’s binocular comfort.
This absence of complaint is also the defining characteristic of a favored industry metric of satisfaction called 20/Happy. However, today there are reasons for both practitioner and patient to be less than happy with 20/Happy. New and advanced lens and assessment technologies have entered the market whose raison d’etre is all about achieving comfortable binocular vision. At the same time, opticians are becoming aware of how choices in lens design, placement and frame style can either complement binocular vision problems or compound them—especially when dealing with a disparate prescription. Therefore, I respectfully submit that nothing breeds both complacency and shortchanges wearer satisfaction more than being satisfied with 20/Happy. While patients do, given enough time, eventually adapt to most changes in Rx or glasses, the most important question now facing every eyecare professional is if they should continue to be happy with 20/Happy.
WHY WEARERS
SUFFER IN SILENCE
The assessment of an individual’s tolerance to binocular issues arising from a disparate Rx is not usually performed within a typical eye exam. The reasons for this are not surprising:
- Much of the testing time in a conventional eye exam is primarily centered on discovering optimal acuity and examining for disease and pathologies.
- Accommodative balance testing, the most common of which is the Duo Chrome test, is done at the end of subjective acuity testing—a time when the patient is fatigued from making finer distinctions, most of the time with declining confidence. The Duo Chrome test itself is often difficult for patients to understand, and it is commonly overlooked when schedules are booked too tight.
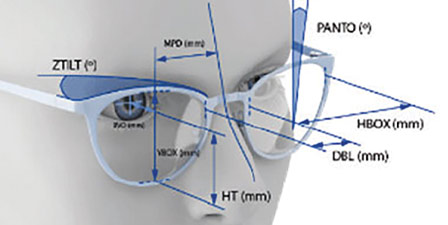
- Rarely is a routine calculation performed to assess for how a disparate Rx would impact binocularity away from the optical center. It is expected that the optician filling the Rx would naturally arrive at a spectacle design that would not aggravate gaze alignment issues—known as anisophoria—or any image size issues that should be better managed in any pair of glasses, let alone those with a disparate Rx.
- Like children with vision issues, adults with binocular vision issues are often not directly aware of the causes behind symptoms of fatigue, blurry vision or headache. Further, even adults can be less capable of articulating or dissecting exactly what they are experiencing. Most end up attributing these symptoms to the stresses in their daily lives or the cumulative impact of daylong computer and phone use.
- The symptoms that accompany compromised binocular vision or poor eye alignment include headache, dizziness, eye strain, neck and shoulder pain, light sensitivity and even dry eye, which may partially explain why ECPs are seeing more and more cases of dry eye.
But the differing amounts of image size and prismatic effects encountered while wearing a disparate Rx—known as static magnification and dynamic magnification—remain insidiously impactful on binocular function and comfort. Even in a single vision pair, the wearer rarely locks their gaze to the area around the OC, which reduces the effects of dynamic magnification and moves their head around like an owl. In multifocals and progressives, the problems multiply, because these lenses require the eyes to linger in the reading zone of the lenses, an area clearly removed from the distance optical center and naturally more affected by the increased amount of dynamic magnification residing there. And all of the above assume the wearer has no phorias or other alignment deficiency that would affect binocularity. If they do, achieving comfortable binocular comfort escalates to an even greater challenge.
THE BENEFITS OF BINOCULARITY
“Two eyes are better than one,” the old saying goes. Let’s take a quick peek at the advantages of having two eyes:
- The brain can use the signal from both eyes to improve the signal-to-noise ratio over that from the image of one eye. This is called binocular summation. Improved threshold luminance detection of a magnitude or more and an increase of up to 40 percent greater image contrast is possible when using two eyes.
- Object distance and surface depth are both improved as a result of stereopsis—the formation of a signal image from two disparate eye perspectives.
- The actual field of view seen by two forward-facing eyes is greater than that of one eye alone, due to monocular field overlap.
- Binocular vision, providing improved depth perception, aids in locomotion, grasping, catching and navigating over uneven terrain.
- When both eyes work together optimally, reading speed and comprehension are possible at much higher performance levels than when an individual’s eyes are not working as a team.
All of the above is excellent motivation for ECPs in order to focus on prioritizing the benefits of comfortable binocular vision.
THE BENEFITS OF
EYE DOMINANCE
Nature has evolved our visual system to make continual choices as to when, where and how to prioritize the integrated visual signal from both eyes versus just one. For example, the parallax created by the separation between our two forward-facing eyes delivers two slightly different perspectives that when combined in the brain, give us the benefit of a single, three-dimensional viewpoint. This combined perspective is referred to as our “cyclopean” eye: a viewpoint presented as if we had a single eye in the middle of our forehead. For a singular binocular image to be properly created from two mildly disparate eye perspectives, the eyes must individually align to the object of regard and map the object to corresponding image points on both retinas. This means that any other object not located on this object’s fixation plane—called the horopter—will end up being seen as doubled, depending on how far removed from the horopter the object points are located. Naturally, all objects located at infinity will have a horopter located there as well.
When an object not lying on the horopter has to be followed, the brain quickly shifts emphasis to the dominant eye for optimal tracking. But the brain will also alternate tracking back to both eyes, depending on the trajectory of the object being followed. This constant handoff in eye tracking is meant to happen seamlessly, from moment to moment. Clearly, any impediment to the proper binocular functioning of the eyes will have significant consequences. In many cases, getting both eyes to work together will benefit from a program of tailored vision therapy, supervised by a trained optometrist.
For optimal binocular vision, object points need to be equally mapped on each retina—a condition referred to as iso-disparate. When the eyes are pointing and focusing together—known as iso-vergent—the object’s location and distance from each eye is proper. Therefore, any disparities in either eye alignment or focus and refractive error can interrupt or impede comfortable binocular vision. This includes misalignments arising from induced disparities in a pair of improperly designed or centered pair of glasses.
THE OPTICIAN’S BV ROLE:
DO NO HARM
Dispensers are trained from day one to respect the Rx, i.e.., to fill it with absolute fidelity to the prescriber’s numbers, with tolerance judgments guided by the latest ANSI standards. But opticians sometimes wonder if they should be modifying the prescription numbers as they see fit. The problem here is how any optician would know the prescriber’s intent behind the prescription numbers, which when done properly, presents a carefully crafted balance between acuity, comfort and utility tailored for that patient. And nowhere is respect for this more important than in prescriptions for individuals with binocular vision disorders.
Even Rxs with no values entered into the prism boxes tell the dispenser little about the true binocular state of that patient. With this in mind, along with the mandate to adhere to the Rx as written, I think it is irresponsible for dispensers today to lack awareness of or sensitivity to how the design choices they make can unfavorably impact binocular vision. To be sure, there’s always a lot of talk on optical social media about the negative effects of peripheral or oblique astigmatism, or the impact of low abbe materials on perceived image quality. But absent are discussions of how to optimize disparate prescriptions or the challenge of fusing differing retinal image sizes. Even less commonly discussed is how disparate prescriptions create variable prism effects in areas away from the OC. These effects are present in prescriptions as mild as plano cylinders with oblique axes, but rare is the discussion of the best lens choices an optician could make for them. Even the most schooled optician may not be sensitive to off-center prismatic and image size effects, except when the Rx is “on fire!” meaning a disparity exceeding 3 to 4 diopters. And even then, most dispensers think of nothing more than using finished stock lenses and using an OC height to optimize the optics. Sure, some opticians are calculating image size at the major reference point and doing their best to minimize the negative impact of aniseikonia. Still others think using the old sledgehammer approach of adding slab off prism in the reading zone is the end of their binocular responsibilities. Particularly today, it seems surprising that most optician training remains deficient in understanding all that can be done to alleviate the compounding of binocular issues. With all the new and novel BV technologies entering the market, opticians should always be recommending lens choices that “do no harm.” (See sidebar: “New BV Technologies That Matter”)
DON’T OVERLOOK VISION THERAPY
Separate from corrections with glasses, many binocular vision issues are often better addressed through the services of a certified Therapeutic Vision Therapist. Remember: A vision processing disorder is very different from a visual acuity deficiency—all the more reasons to be current with the latest visual assessment tools and technologies.
Vision therapy encompasses many areas, including but not limited to:
- Visual acquisition: visual intake and eye tracking.
- Visual sensory motor: anomalies in the Lateral Geniculate Nucleas, or LGN and visual integration, which is vision’s ability to work with other sensory modalities.
- Visual perception: a term that encompasses vision analysis, visual thinking, visual logic, visual manipulation and visualization.
New BV Technologies That Matter
An isotropic prescription—that is, an Rx of nearly equal refractive power between the eyes—clearly represents a situation that poses the least amount of potential binocular issues with carelessly chosen glasses. But as the prescription between the eyes becomes more disparate or contains even minor amounts of oblique astigmatism, two situations immediately arise: One where retinal image size notably differs between the eyes, and the other where prismatic effects arising from differing lens powers challenge binocular comfort as the eyes gaze to lens regions beyond the actual optical center.
Clearly the amount of impact on wearer comfort depends on the degree of the Rx difference, together with wearer tolerance. And we have established thresholds regarding the amount of acceptable image size and prismatic imbalance derived from data averaged across the larger population. But left out of these accepted thresholds is the exact knowledge of acceptable tolerance—without symptom—for any specific individual. And that’s where today’s newest lens and assessment technologies can help patient comfort and allow ECPs to shine!
With this in mind, ECPs should be thinking more about binocular vision and aniseikonic issues. Here’s why:
- There are several new and more advanced binocular vision lens solutions now on the market that globally manage and optimize the entire lens surface, rather than a single location.
- New assessment technologies now exist offering quicker and more precise determination of when either overt or latent binocular vision issues are present. Traditionally, assessment of binocular vision disorders was based primarily on a doctor’s subjective evaluation.
- Binocular vision disorders, because of the stresses they place on our vision, appear to be a possible contributing factor for the increases in the amount of dry eye disease occurring.
With both aniseikonia and BV disorders, precision in analysis and treatment is the key to significantly improving patient comfort. Shaw Lens, Neurolens and RightEye are three companies leading the way to both better patient outcomes and increased practitioner confidence and satisfaction. Let’s look at each of these company’s offerings.
SHAW LENS
“Aniseikonia Solved!” is the banner that greets you on the landing page of Shaw Lens. But is that what is truly new from Dr. Peter Shaw’s company? After all, the basic formulae for calculating the lenses needed to help equalize retinal image sizes have been known and taught to every optometrist and optician. The differences with Shaw Lenses are manifold:
- Shaw Lens calculates the compensations needed in a global, rather than local manner. There’s more going on across a lens surface than just at the major reference point where the eyes are pointing straight ahead.
- Shaw Lens uses a proprietary algorithm, based in large part on the pioneering foundational work of Arthur Remole, OD, to optimize the entire lens surface for disparities in static and dynamic prism considerations and magnification.
- Shaw Lens employs a top tier, free form progressive lens design as the basis for their proprietary compensations. Because of this, Shaw aniseikonic lenses can be easily updated to the latest progressive lens advancements.
- Shaw Lenses work best with a properly chosen frame—one that places the pupil within 4 mm of the midpoint of the lens. “If your patients want the best optics and visual comfort, then fitting with a skilled and experienced dispensing professional is a must,” says Dr. Shaw.
Dr. Shaw offers a few insights on managing binocular vision:
- Using the shorter corridors available in today’s advanced free form lenses no longer comes with the optical penalty of unwearable astigmatism. Shorter corridors allow for more modest eye depression angles to reach the full add reading zone. Shorter corridors reduce the amplitude of the imbalances being addressed by his design.
- Although not related just to aniseikonia per se, Shaw Lens avoids the use of polycarbonate as a material substrate, favoring 1.60 index for its better abbe value and 1.67 index for its ability to create the higher surface powers needed to optimize image size.
- When reviewing an Rx for use with Shaw’s optimizing process, don’t forget that smaller Rx disparities between the eyes are often as important as larger disparities. “Wearers with smaller Rx differences have been typically overlooked by ECPs, because they often don’t see the need. But these same patients are using both eyes far more than people with larger disparities, whose binocular vision is often compromised by moderate to greater eye suppression. The patients with smaller disparities are often the individuals who enjoy the greatest immediate relief and benefit from our advanced aniseikonic approach.”
- The best frame shape and size for a Shaw lens is often the best frame choice for any more challenging Rx.
- Just like any Rx, some individual tweaking after dispensing may be required.
Shaw Lenses are available from independent labs. Check with your local lab.
NEUROLENS
Aric Plumley is the engineer and driving force behind the Neurolens technology. With many people having to work all day with various display technologies ranging from phone to tablet to desktop, more and more people find themselves suffering from headaches, dizziness and head and neck strain caused by often undiagnosed minor eye alignments. Using the Neurolens Analyzer, which can repeatably and precisely measure minor misalignments, and in concert with the advanced variable and individually tailored prism referred to as “contoured prism” in their single vision and progressive lenses, Neurolens promises consumers a new and novel solution for these minor misalignments.
The Neurolens experience starts with the patient completing an intake form designed to reveal common but often overlooked symptoms of visual distress. Today, I think consumers naturally dismiss all sorts of visual discomfort, attributing it to the stress of their job or life. But there’s another factor why the public tolerates stress: It’s part of today’s work culture to stay the course and “tough it out.” Neurolens asks: “Why do so when relief is in sight”?
Next up is assessment with the Neurolens Measurement Device. Unlike classic subjective refraction, there’s no hard-to-discern, confusing or difficult choices for a prospective Neurolens candidate to make. This alone separates the Neurolens experience from the traditional subjective binocular vision testing done by an individual doctor.
Finally… the Neurolenses are ordered and dispensed. The uniqueness of Neurolens resides in the ability to offer precise prism that can be varied or “contoured” within the convenience of a single pair of glasses. Rather than a single global prism value that may not be optimum for all distances, Neurolens recognizes that alignment demands may vary from distance to intermediate and near tasks, and their unique assessment and lenses deliver an individually tailored solution.
RIGHTEYE
The RightEye Automated Sensorimotor Exam System is a new, more precise and more comprehensive way of assessing binocular vision disfunction, or BVD. Coming from a company that specializes in advanced eye tracking, the RightEye Exam assessment is a one-minute objective system yielding data rich information revealing all types of misalignments that can impact the natural teaming function between the eyes. Because of its subjective nature, RightEye posits that many misalignments may go undiagnosed with traditional Four H and Worth 4 Dot tests, as these tests are long and typically done at the end of all the exams, when the patient is at their most fatigued. RightEye cites that the Dizziness and Headache Optometry Center has found that 56 percent of the population demonstrates symptomatic effects, including headaches, dizziness, fatigue, upper body pain, and compromised school and work performance arising from deficiencies in convergence, eye tracking and reading comprehension. Further, 1 in 6 individuals suffers from some degree of abnormal convergence insufficiency. The one minute RightEye exam may be just the ticket to both helping your patients and differentiating your practice.
Read Part Two of “The New 20/Happy” »
Contributing editor Barry Santini is a New York State licensed optician and contact lens fitter with Long Island Opticians in Seaford, N.Y.