ABSTRACT
High blood pressure is not only bad for your cardiovascular system but for your eyes and vision as well. At least 50 million Americans suffer from hypertension. Uncontrolled high blood pressure increases the risk of serious health problems, including heart disease, stroke, and hypertensive retinopathy. The danger posed by hypertension is that blood pressure can be high for years without a patient noticing any symptoms. Hypertension can be diagnosed by an optometrist and by a primary care physician and controlled with medication and diet (Kovach, Schwartz, Schneider & Rosen, 2012). Concentrating on a review of recent literature, this paper focuses upon the broad spectrum of ocular problems caused by hypertension.
INTRODUCTION
This paper aims to enhance the understanding of hypertensive retinopathy and its relationship to high blood pressure since high blood pressure (hypertension) affects approximately one-third of adults in the United States. Hypertension is an increase in blood pressure that affects many organs in the body. What most people don't realize is that hypertension can occur in your eyes. This is called intraocular pressure. Ocular hypertension usually occurs when the pressure inside the eye is higher than normal. An increase in pressure in the eyes will damage the walls of the small retinal and optic nerve arteries, which can lead to vision loss over time (Schwartz, Schneider & Mieler, 2013). Uncontrolled high blood pressure will eventually cause severe health problems such as cardiovascular disease, stroke, ocular retinopathy and other ocular diseases. Reed (2014) states that the most common ocular problems arising from hypertension are hypertensive retinopathy, retinal vascular occlusions, cranial nerve palsies and optic neuropathy. The danger of hypertension is that a patient can be unaware of the disease since physical signs may not always be apparent. Therefore, it is imperative that hypertension not be ignored by the optometrist since helping the patient manage eyecare health is of utmost importance. The optometrist should obtain the most recent information about this disease in order to be aware of the detrimental effect undiagnosed and/or uncontrolled hypertension can have upon the vision of a patient (Schwartz, Schneider & Mieler, 2013).
DEFINITION OF HYPERTENSION
High blood pressure is a condition in which the force of the blood against the artery walls is too high. Blood pressure is determined by the amount of blood the heart pumps and the amount of resistance to blood flow in the arteries as determined by a blood pressure reading taken with a sphygmomanometer. The more blood the heart pumps and the narrower the arteries, the higher the blood pressure. The systolic top number is a measure of pressure inside the arteries as the heart beats. The diastolic second number indicates the pressure between beats when the heart is resting (Mayo Clinic, 2011). One or both of these numbers can be too high. Kovach, Schwartz, Schneider & Rosen (2012) state that a normal blood pressure is 120 over 80. High blood pressure is a repeated systolic pressure above 140 or a diastolic pressure above 90. According to recently posted findings by the American Heart Association (2014) a pre-hypertension category is a systolic blood pressure of 120-139 and a diastolic pressure of 80-89. Patients in this category are more likely to be instructed to modify their diet and increase their exercise level rather than being placed on antihypertensive therapy. The American Heart Association website offers an interactive tool to help patients reduce their blood pressure through lifestyle changes. The Mayo Clinic (2011) blood pressure guidelines for patients under age 60, suggests that blood pressure should be below 140/90 and for those 60 or older, less than 150/90. Medications known as antihypertensives are available by prescription to lower high blood pressure. Physicians have a variety of classes of high blood pressure medications to choose from to treat their patients. They include a number of different drugs from which to select starting treatment for hypertension without limiting preference to a single class as done in the previous guidelines (Mayo Clinic, 2011).
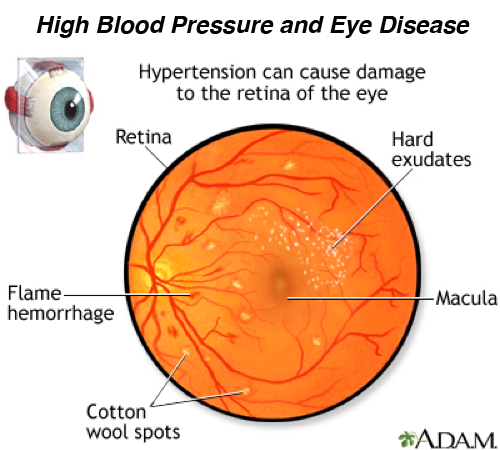
Hypertension that is uncontrolled can cause hypertensive retinopathy, which is a severe detrimental condition that affects vision. The retina is the lining of the back of the eye and has delicate blood vessels lining on top of it and below. The retina can be affected by many medical conditions and eye diseases. If high blood pressure is not well controlled, changes can happen in the retinal blood vessels. These changes are called hypertensive retinopathy (Pavan-Langston, 2008).
DIAGNOSIS OF RETINAL PROBLEMS
Although today's media raises public awareness of the physical, social, and financial ramifications of careless dietary habits and lack of ample physical activity, obesity rates are extremely high in the American population. Obesity has become one of the leading causes of high blood pressure and Type II diabetes. High blood pressure, Type I (juvenile onset) diabetes and Type II (adult onset) diabetes are diseases that can have a detrimental effect upon vision (Fryer & Carroll, 2014). According to Kimberly Reed, OD (2014) until recently, optometrists did not consider obesity as a risk factor in the diagnosis of severe ocular conditions. Reed (2014) states that obesity can cause detrimental health problems such as hypertension and diabetes and those diseases may lead to ocular problems. Reed (2014) concurs with the American Optometric Association Practice Guidelines for Comprehensive Adult Eye and Vision Examination, that patients with diabetes and/or hypertension are at risk for significant ocular complications. Those patients should undergo a comprehensive evaluation annually, whereas people who are healthy need to be evaluated every two years.
A study done by Zheng, Nguyen, Armitage, Vingrys, & Bui (2012) has determined that blood pressure plays an important role in glaucoma. The authors state that a number of large scale epidemiological trials found a lower risk of glaucoma in people with high blood pressure, whereas other studies found the opposite. Therefore, the authors suggest that the influence of systemic hypertension on glaucoma needs further evaluation and a patient's blood pressure needs to be monitored.
According to Garibaldi (2013) every patient deserves the benefit of a comprehensive evaluation with attention paid to determine the presence of symptoms of hypertensive retinopathy such as decreased vision, distortion of vision and loss of color vision. Pavan-Langston (2008) states that the optometrist should take the patient's complete medical history, including: family medical history, past illnesses and surgeries, allergies, medications, symptoms or complaints and a blood pressure reading should be taken. In addition, the following exams and tests should be performed by the optometrist to determine if hypertensive retinopathy does or does not exist: A dilated fundus exam will allow the optometrist to view the retina to determine if hypertension has affected the retina. This is done using an ophthalmoscope. The doctor can see narrowing of blood vessels, and signs that fluid has leaked from blood vessels (Trottini & Tolud, 2013).
An exam using a slit lamp with the help of the Digital Wide Field Lens (Volk Optical) or through binocular indirect ophthalmoscopy to look at the back of the eye. Both techniques allow the doctor to view the blood vessels, but can also help discern differences in elevation and/or edema (Trottini & Tolud, 2013).
An exam using Mydriatic drops, to enlarge and dilate the pupils to look into the back of the eye (Trottini &,Tolud, 2013).
A visual field test can help diagnose the extent of hypertensive retinopathy. This instrument presents spots of light to a patient in order to determine which parts of the retina are not seeing properly. The visual field test can also detect certain visual field losses that are predictable in hypertensive patients who have had a stroke. Although the retina and optic nerve may look fine, the visual field test is a test the doctor can use to determine which part of the brain has been affected by a stroke. This test aids in the detection of: optic nerve diseases, glaucoma damage, diseases affecting visual pathways within the brain, eyelid conditions and to measure central and peripheral vision (Garibaldi, 2013).
A Fluorescein Angiography test examines the vasculature of the retina. This test requires the injection of fluorescein into the vein of a patient. The retina is viewed through a dilated pupil as the fluorescein makes its way through the blood vessels of the retina. A camera equipped with special lenses and filters, takes picture of the retina. This test can determine the extent of hypertensive retinopathy by finding any hemorrhages or blockages of the blood vessels as well as any swelling or edema of the retina or optic nerve (Pavan-Langston, 2008).
OCULAR COMPLICATIONS OF HYPERTENSION
High blood pressure can damage blood vessels in the retina. Hypertensive retinopathy is damage to the retina due to a systemic blood pressure higher than the eye can tolerate. The retina is the layer of tissue that lines the back part of the eye. The retina changes light and images into nerve signals that are sent to the brain. The retina has infinite delicate blood vessels that can be affected by various medical conditions and eye diseases. Detrimental changes in the retinal blood vessels can occur when high blood pressure is not controlled, which may cause a loss of vision that can become permanent. The higher the blood pressure and the longer it has been high, the more severe the damage. Symptoms may include: double vision or dim vision, headaches, visual disturbances, and sometimes sudden vision loss. Sudden symptoms can be a medical emergency. Unfortunately, most people with hypertensive retinopathy do not have symptoms until late in the disease (Garibaldi, 2013). When patients with elevated blood pressure are diagnosed with hypertensive retinopathy, the result is a series of retinal microvascular changes. These changes can result in the following:
Retinal arteriolar narrowing - a known result of hypertension that can predict cardiovascular mortality in adults (Reed & Shah, 2014, 2014).
Arteriovenous nicking - a small artery (arteriole) is seen crossing a small vein (venule), which results in the compression of the vein with bulging on either side of the crossing (Reed & Bhargava, 2014, 2012).
Retinal hemorrhages - the abnormal bleeding of the blood vessels in the retina (Shah, 2014).
Retinal microaneurysms - a tiny area of blood protruding from an artery or vein in the back of the eye. These protrusions may open and leak blood into the retinal tissue surrounding it. (Shah, 2014).
Macular edema - occurs when fluid leaks from the retina's blood vessels and collects on or under the macula of the eye causing it to swell and thicken. The macula is responsible for central or pinpoint vision. Macular edema affects clear vision (Bhargava, 2012).
Optic disc edema – a swelling of the optic disc (papilledema) can be caused by a number of conditions. Severely elevated systemic blood pressure causes this swelling. It can be indicative of impending stroke or/and possible death. The optic disk is a small oval-shaped area on the retina marking the site of entrance into the eyeball of the optic nerve (Bhargava, 2012).
According to Schwartz, Schneider & Mieler (2013) chronic elevated blood pressure can lead to hypertensive choroidopathy. This condition is seen in young patients who have pliable blood vessels that are not sclerotic from a long period of hypertension. The authors describe the choroid, which is also known as the choroidea or choroid coat, as the vascular layer of the eye, containing connective tissue which lies between the retina and the sclera. They further state that retinal microvascular signs of hypertension can be seen in other systemic and ocular conditions. Therefore, further medical examination of the patient is necessary in order to rule out diseases that are not the result of hypertension.
STAGES OF HYPERTENSIVE RETINOPATHY
Larsen, Soliman, Kern, and Mohr (2007) state that there are changes to the retina, as a result of systemic hypertension beginning with narrowing of the retinal arteries. As the narrowing progresses, the retinal arteries start to bleed in the form of flame hemorrhages. Compression of the veins occurs at the points where the arteries cross the retinal veins, called A/V nicking. Total occlusions and large amounts of bleeding in the back of the eye occur. Irreversible retinal damage and vision loss can result. As hypertensive retinopathy progresses, areas of the retina can become ischemic. This occurs when there is an inadequate supply of blood to an organ as a result of an obstructed blood flow and a lack of oxygen. Cotton wool spots develop on the retina in the areas of ischemia. The cotton wool spots typically show advanced hypertensive damage. Larsen, Soliman, Kern, and Mohr (2007) grade the degree of retina damage (retinopathy) on a scale of 1 to 4.
- At grade 1, the patient may not have symptoms.
- In between grades 1 and 4, there are a number of changes in the blood vessels, leaking from blood vessels, and swelling in other parts of the retina.
- Grade 4 retinopathy includes swelling of the optic nerve and of the visual center of the retina (macula). This swelling can cause decreased vision (pp. 291-391).
Wolf, Klesert, and Schachat (2007) give a more detailed classification of hypertensive vascular fundus changes. The authors believe this detailed classification is important for scientific reasons, but may not be as practical for the clinical management of systemic hypertension. However, they believe that the vascular changes in systemic hypertension (stages I and II) and hypertensive retinopathy (stages III and IV) are extremely important for the management of arterial hypertension. For the purpose of clarification for the reader of this paper, the stages are listed as follows:
Stage 1- Brighter reflexes on arterioles
- Vascular distension and tortuosity ( seen as silver wiring)
- No parenchymal changes
- Arteriosclerosis of variable severity
- Hypovolemic hypertension
- Arterioles generalized narrowing in caliber
- Circumscribed areas of narrowed caliber (known as AV nicking or nipping)
- Increase and irregular reflexes
- Paramacular venules distended tortuous sign of venous stasis
- Isolated capillaries visible (capillary ectasia) in central retina and on the optic disk
- Hyperemia on the optic disk
- Fine retinal hemorrhages
- Generalized narrowing of the arterioles
- Arterioles appearing thin and threadlike in places
- Segmental or rosary like constrictions
- Bright and irregular reflexes
- Siegrist's streaks and obliterated vessels
- Cotton wool spots
- Hard exudates macular star
- Retinal hemorrages
- Optic disk edema
- Changes as in stage 3 covering the entire fundus
- Bilateral papilledema (swelling of the optic disk)
- Retinal edema
- Exudative retinal detachment (p.690).
Wolf, Klesert, and Schachat (2007) explain that stage 4 retinopathy includes swelling of the optic nerve and of the visual center of the retina (macula) and that this swelling can cause decreased vision. They state that the retina may recover once blood pressure is controlled. However, they further state some patients with stage 4 retinopathy will have permanent damage to the optic nerve or macula. Also, patients with stage 4 (severe retinopathy) can often have heart and kidney problems due to high blood pressure. These patients are at higher risk for stroke and need to be monitored.
MANAGEMENT
Optometric patient management should include: accurate documentation in the patient's chart, inform the primary care physician about the patient's ocular condition, recommend that the patient adhere to the treatment prescribed by both the primary and eyecare doctors and educate the patient about the ocular condition (Pavan-Langston 2008). Controlling high blood pressure prevents changes in the blood vessels of the eye, as well as in other organs like the heart, kidneys, and brain. Therefore, controlling high blood pressure is the only treatment for hypertensive retinopathy. The patient needs to follow a healthy lifestyle and adhere to the appropriate medical drug treatment (Reed, 2014).
CONCLUSION
Hypertension is prevalent among adults in the United States. When a patient is obese, has high blood pressure, diabetes, high cholesterol levels, or smokes, there is a higher risk of eye damage and vision loss (Reed, 2014). Hypertension increases the risk of problems to the retina such as: Ischemic optic neuropathy (damage to the nerves in the eye due to poor blood flow), retinal artery occlusion (blockage of the blood supply in the arteries to the retina), retinal vein occlusion (blockage of the veins that carry blood away from the retinas of retinal diseases), diabetic retinopathy, and anterior ischemic optic neuropathy. Hypertensive retinopathy is associated with increased risks of stroke, cognitive impairment, and cardiovascular death (Schwartz, Schneider & Mieler, 2013). Most patients in the early stages of hypertensive retinopathy do not report experiencing any symptoms. Therefore, it is extremely important for at risk hypertensive patients to have regularly scheduled comprehensive eye exams (Kovach, Schwartz, Schneider & Rosen, 2012). It is imperative that the primary care physician and optometrist emphasize to the patient that blood pressure be kept under control in order to prevent the onset of hypertensive retinopathy.
Damage to the retina from high blood pressure is called hypertensive retinopathy. It occurs as the existing high blood pressure causes changes to the microvasculature of the retina. Some of the first findings in the disease are flame hemorrhages and cotton wool spots. As hypertensive retinopathy progressives, hard exudates can appear around the macula along with swelling of the macula and the optic nerve, causing impairment of vision. In severe cases permanent damage to the optic nerve or macula can occur.
Kovach, J., Schwartz, S., Schneider, S., Rosen, R. ( 2012). Systemic hypertension and the eye. In: Tasman W., Jaeger E. (Eds.), Duane's Ophthalmology. 16th ed. (Chapter 13). Philadelphia, Pa: Lippincott Williams & Wilkins.
References
American Heart Association. About High Blood Pressure. February 21, 2014. Retrieved from http://www.heart.org/HEARTORG/Conditions/high bloodpressure/About-High-Blood-Pressure UMC 002050 Article.jsp
Bhargava, M., Ikram, M., & Wong, T. (2012). How Does Hypertension Affect Your Eyes? Journal Of Human Hypertension, 26(2), 71-83.
Fryer, C., Carroll, O. (2014). National Center for Health Statistics. Prevalence of Obesity and Extreme Obesity Among Adults: United States, Trends 1960-1962 through 2009-2010. Retrieved from: http://www.cdc.gov/nchs/data/hestat/obesity/adult-09-10/obesity-adult-9-10.htm
Garibaldi, D. High Blood Pressure and Retina Problems. (2013). CRS - Adult Health Advisor:1:1.
Kovach, J., Schwartz, S., Schneider, S., Rosen, R. ( 2012). Systemic Hypertension and the Eye. In: Tasman W., Jaeger E. (Eds.), Duane's Ophthalmology. 16th ed. (Chapter 13). Philadelphia, Pa: Lippincott Williams & Wilkins.
Larsen, M., Soliman, W., Kern, T., Mohr, S. (2007).Grading of Diabetic Retinopathy. A. Joussen, T. Gardner, B. Kirchhof, S. Ryan (Eds). In Retinal Vascular Disease (pp. 291-391). Berlin, New York: Springer-Verlag.
Mayo Clinic Staff. High Blood Pressure Dangers: Hypertension's effects on the body. Feb. 18, 2011. Retrieved from:
http://www.mayoclinic.com/health/high-blood-pressure/HI00062/NSECTIONGROUP=2
Pavan-Langston, D. (2008). Manual of Ocular Diagnosis and Therapy. 6th ed. Philadelphia, Pa: Lippincott Williams & Wilkins, Chapters 1, 8.
Reed, K.(2014) Obesity Counseling is Within our Scope. Review Of Optometry:15.(3), 52-59.
Schwartz, S., Schneider, S., Mieler,W. (2013). Retinal and Choroidal Manifestations of Systemic Hypertension. In J. Arevalo (Ed.), Retinal and Choroidal Manifestations of Selected Systemic Disease (pp.387-416). New York: Springer.
Shah, V. (2014). Retina/Vitreous. Retrieved from: http://eyewiki.org/Category:Retina/Vitreous Trottini, M., Tolud,C. (2013). Essential Elements of the Retinal Exam. Review of Optometry: 150 (6), 50-55.
Wolf, S., Klesert, T., Schachat, A. (2007). Hypertensive Retinopathies: General Basics of Hypertensive Retinopathy. In Joussen, M., & Gardner, T. (Eds.), Retinal Vascular Disease (pp. 688-699). New York: Springer.
Zheng, H., Nguyen, C., Armitage, J., Vingrys, A., & Bui, B. (2012). Blood Pressure Modifies Retinal Susceptibility to Intraocular Pressure Elevation. Plos ONE, 7(2), 1-9.

Benjamin Betines, a student at Raritan Valley Community College in Branchburg, New Jersey pursuing an Ophthalmic Science (Opticianry) Associate of Applied Science degree. He is currently employed as an Apprentice Ophthalmic Dispenser in New Jersey.