By Kai Rands
ECPs are often taught that binocular vision disorders can be addressed by applying prism uniformly across lenses. Recent research suggests that contoured prism may alleviate symptoms such as asthenopia, headaches and neck pain among those with even small eye misalignments. Contoured prism varies the amount of prism across the lens to address the viewer’s prismatic needs at different distances.
As ECPs, we can better enhance patients’ binocular vision functioning as well as alleviate associated discomfort when we know when and how to leverage prism with patients. Let’s take a deeper look at this fundamental principle of ophthalmic optics and see how we can harness its power.
BINOCULAR SENSORY PERCEPTION
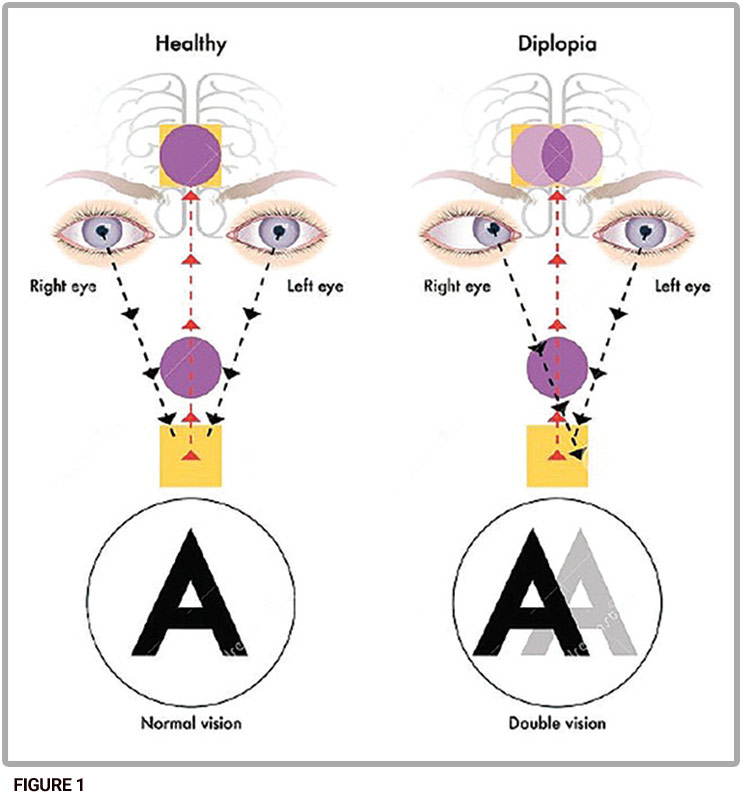
Binocular vision affords a larger field of view, compensates for the optic disc scotoma and enhances depth perception as compared to vision with a single eye. These benefits rely on the interpupillary distance. Since the two eyes are separated horizontally on the face, the light reflecting off objects and entering the eye form slightly different images, a phenomenon referred to as retinal disparity. Yet, those with binocular vision see a single image. This conundrum has fascinated thinkers throughout the ages.
Macular perception is the most basic level of sensory status in binocular vision. The visual axis of each eye connects the object, through the center of rotation of the eye, to the fovea. Fusion, the next grade of sensory status, occurs not within the eye but further along the visual pathways and results in the perception of a single image. In stereopsis, the highest grade of binocular sensory perception, the neural circuitry in the visual pathways uses complex computations to detect the location of objects in three-dimensional space.
Binocular sensory perception requires the eyes to converge or diverge so that the visual axes continue to connect objects at different distances to the fovea of each eye. This is accomplished by the extraocular muscles. For convergence, the medial rectus muscles contract while the lateral rectus muscles relax. In divergence, the lateral rectus muscles contract while the medial rectus muscles relax. Vergence responses must coordinate with accommodation to keep the image clear. A common measure of this relationship is the accommodative convergence to accommodation ratio, AC/A.
BINOCULAR VISION
DYSFUNCTIONS AND
MEASUREMENT TECHNIQUES
Binocular Vision Dysfunction can occur at any point in coordinating eye movement, accommodation and sensory processing. Phorias and tropias involve misalignment of the visual axes. A manifest tropia is always apparent. Intermittent tropias are only apparent some of the time. Phorias last a very short time. Researchers and clinicians have developed scales to rate eye turn duration from pure phoria all the way up to manifest tropia, according to Clinical Management of Binocular Vision by Mitchell Scheiman and Bruce Wick.
Clinicians also use prisms to determine the magnitude of a phoria or tropia. The general idea is to use high prism to dissociate the images between the eyes. In other words, the clinician purposefully induces diplopia. Dissociating the images allows the clinician to observe the behavior of the eyes independently. Dr. Sheiman and Dr. Wick describe the von Graefe technique that uses this approach. The left eye views an optotype (e.g., letter on a Snellen chart) through a horizontal prism and the right eye views through a vertical prism. The horizontal prism is approximately 10^ to 12^BI and the vertical prism is about 6^BD. To measure the horizontal deviation, the clinician adjusts the magnitude of the horizontal prism until the patient says that the top and bottom images of the optotype align. This measurement technique is often performed at distance and near because the magnitude of the phoria is typically different at these distances. Most people tend to have a small exophoria. The expected mean distance horizontal deviation for adults is 1 prism diopter exophoria with a standard deviation of +/-1 prism diopter. So, approximately 68 percent of the population has a horizontal deviation of 0 prism diopters (orthophoria) to 2 prism diopters exophoria based on the statistical normal distribution. For near, the expected mean horizontal deviation for adults is 3 prism diopters exophoria with a standard deviation of +/- 3 prism diopters. So, approximately 68 percent of adults have 0 prism diopters (orthophoria) to 6 prism diopters exophoria at near.
When fixating on an object, two forces are in play. One force moves the visual axes according to the phoria; the other force moves the visual axes toward the object through the vergence response. Fixation disparity is the difference between the visual target vergence angle (the angle created by connecting the eyes to the target) and the viewer’s vergence angle under binocular viewing. In other words, measures of fixation disparity indicate the viewer’s ability to compensate for a phoria.
BINOCULAR FUNCTION, PAIN
AND DISCOMFORT
What happens if a patient’s phoria is within the typical range for distance but outside the range at near or vice versa? In this case, the patient’s eyes are converging too much (convergence excess) or too little (convergence insufficiency), or diverging too much (divergence excess) or too little (divergence insufficiency). These conditions are associated with symptoms such as asthenopia, headaches, intermittent blur or diplopia, burning and tearing. Researchers are currently investigating whether these symptoms also arise from smaller, more typical phorias. The trigeminal nerve is a cranial nerve that transmits sensory information related to temperature, touch and pain from the face, including the eyes, to the trigeminal nucleus, which projects to other parts of the nervous system. One theory under investigation associates small eye misalignments with a broad cluster of symptoms referred to as trigeminal dysphoria. More research is needed to confirm this theory and investigate the mechanisms involved.
UNIFORM WEDGE PRISMS
Using uniform prism is one strategy for addressing the symptoms associated with binocular vision disorders. A prism bends light toward the base and displaces the image toward the apex. When the image appears in a different place, the eye’s visual axis must point in a different direction to maintain fixation on the object. Most simply, we can insert a plano wedge prism into a frame for a patient without a refractive error. In practice, wedge prisms are rarely used for daily use. A lens with uniform base up prism would move the image down toward the apex so the eye would turn down to align with the new location of the image. Uniform base down prism has the opposite effect—the image is displaced up so the eye turns up. Uniform base in prism displaces the image temporally so that the eye turns out and base out prism displaces the image nasally so that the eye turns in. In practice, plano lenses with uniform prism typically have a positive base curve.
OPHTHALMIC LENSES AND PRISM
As we know, non-plano ophthalmic lenses are designed to converge light to correct for hyperopia and diverge light to correct for myopia. To do so, plus lenses are thickest at the optical center and thinner around the edges. In essence, the edges of a plus lens are an apex, and the optical center is a base of a concentric prism. The opposite is true of a minus lens: the edges are a base, and the optical center is the apex. In contrast to the plano prisms described above, the plus and minus lenses also curve at different rates on the front and back surfaces, so the amount of prism changes based on the dioptric power. For spherocylindrical lenses, since the dioptric power changes based on the meridian (as found using the oblique meridian formula), the amount of prism also changes based on the meridian. Prentice’s Rule describes this relationship mathematically. The amount of prism in prism diopters is the product of the dioptric power along the given meridian and the distance from the optical center in centimeters.
PRESCRIBED PRISM
Patients often benefit from prism while still having a refractive error. The lens must do double duty: displace the image and correct the refractive error. One way to accomplish both tasks is to decenter the optical center of a spherical or spherocylindrical lens. Then the patient’s visual axis at primary gaze passes through a point on the lens with the desired amount of prismatic effect. Another option is to surface the lens so that it already combines the spherical or spherocylindrical curvature with uniform prism.
We can use prism to move an image of an object, but in which direction should we move the image? We can take two approaches: Move the image toward the patient’s existing visual axis, or move the patient’s visual axis toward the object. Moving the image toward the patient’s existing visual axis is relieving or therapeutic prism. The prism relieves the need for the extraocular musculature from constantly attempting to fixate an object with both eyes. This can make fusion easier. In this case, the base is placed on the opposite side from the deviation. Moving the visual axis toward the object is adverse prism. To do so, the base is placed in the direction of the deviation. The prism challenges the extraocular musculature to build up the strength and skill to fixate on the object.
NEW MEASUREMENT TECHNIQUES
In October 2023, Neurolens, a company specializing in contoured prism technology, introduced a new virtual reality-based device that measures binocular alignment. Like previous Neurolens measurement devices, the N3 measures phorias at distance and near, fixation disparity and accommodative convergence response, according to a Neurolens blog post. Similar to the von Graefe technique, the N3 uses a dissociative test with non-fusible targets to measure eye misalignment. N3 also measures fixation disparity and the accommodative convergence response.
The N3 guides the patient through the measurement process, which can be conducted in the pretesting area or exam room. After the assessment, while the patient is still immersed in virtual reality, the device demonstrates any misalignment findings to the patient and asks whether the patient would like to discuss the findings with the optometrist.
Tausha Barton, OD, a consultant for Neurolens, began using the N3 in October 2023. Among her first patients were two brothers, ages 9 and 11. After the children completed the testing, the 9-year-old reported “Yeah, it was easy… it said I have an eye misalignment and need special glasses to fix it.” When Dr. Barton looked at the results, she noted that the 19-year-old had exophoria at distance and esophoria at near, an uncommon misalignment. Based on these findings, Dr. Barton asked the mother about the younger boy’s reading performance at school. The screening questionnaire before testing had not revealed any symptoms. Following up on the N3 results exposed a more detailed picture. When asked how the youngest boy was doing in reading, the mother reported that his reading performance was below expectations and that he avoided reading. Dr. Barton suggested that the reading difficulties may be due to eye misalignment at near rather than a learning difference: “If a child’s eyes are uncomfortable, they may avoid things that make them uncomfortable…They don’t have the vocabulary or knowledge that what they are experiencing with words moving on the page or splitting apart is not normal.” One of the children also volunteered that when he is watching TV, the image splits into two. When he blinks a few times, the image returns to a single image. Neurolenses may enhance the children’s quality of life by improving their binocular vision. Dr. Barton prescribed Neurolenses as a solution to improve the boys’ binocular vision.
Ophthalmic optics researchers, suppliers and eyecare professionals continue to master the technology of prisms to move images to their advantage. Technology such as the N3 measurement device and contoured lenses bring precision to binocular function assessment and ophthalmic lens design. As experts in ophthalmic lenses, opticians have an opportunity to be leaders in this process.
CONTOURED PRISM
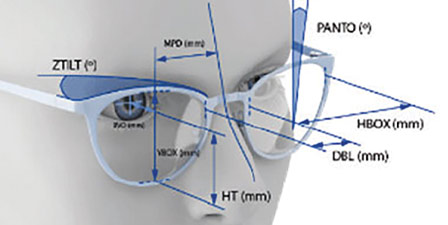
 Opticians specialize in manufacturing and fitting lenses to optimize patients’ visual experience in natural settings. As such, more optical labs such as Cherry Optical Lab are beginning to manufacture contoured prism lenses through freeform digital technology. Dispensing opticians ensure that the eyes and contoured prism lenses work together as a system. Opticians also continue the education begun in the exam room. Patients may not have been exposed to information about binocular vision and eye misalignment in previous settings. Opticians can help patients distinguish between visual acuity and binocular function. Patients may expect lenses with contoured prism to help images to appear clearer so opticians can highlight that the purpose of contoured prism is to counteract eye misalignment and improve symptoms such as headaches and eye strain.
Opticians specialize in manufacturing and fitting lenses to optimize patients’ visual experience in natural settings. As such, more optical labs such as Cherry Optical Lab are beginning to manufacture contoured prism lenses through freeform digital technology. Dispensing opticians ensure that the eyes and contoured prism lenses work together as a system. Opticians also continue the education begun in the exam room. Patients may not have been exposed to information about binocular vision and eye misalignment in previous settings. Opticians can help patients distinguish between visual acuity and binocular function. Patients may expect lenses with contoured prism to help images to appear clearer so opticians can highlight that the purpose of contoured prism is to counteract eye misalignment and improve symptoms such as headaches and eye strain.
The Neurolens measuring devices, including the most recent N3, provide the data needed to produce lenses with contoured prism. Freeform technology precisely contours the lens so that the amount of prism varies to account for eye misalignment differences at distance and near. Since most people have less misalignment at distance than at near, the amount of prism in a contoured lens typically increases gradually from distance to near. Often this is compared to progressive lenses: in progressive lenses, the dioptric power gradually increases from distance to near; in contoured prism, the amount of prism gradually increases from distance to near. Presbyopes may benefit from both progressive lenses and lenses with contoured prism. Neurolenses can combine the gradual increase in dioptric power with the gradual increase in prism to provide both effects.

Dr. Barton told the story of a mother in her 30s who had experienced migraines and neck tension for at least 10 years. The mother’s headaches occurred five to seven days per week. She had tried a variety of treatments including chiropractic, massage, botox injections and antidepressants. The mother was fitted with contoured lenses. The mother reported to Dr. Barton that the night after wearing the Neurolenses was the first night she had gone to bed without neck pain in 10 years.
Neurolens completed a clinical trial of the effect of contoured prism on headache reduction in May 2022. Publications are not yet available on the National Library of Medicine website. Three third-party studies are in process at universities.
–KR
Kai Rands is an optician involved in providing visual aids to those with low vision.