By Sara Bonizio
“My patients are already trying out online eye tests and ordering glasses.”
“Can these remote systems really deliver a proper eye exam?”
“It’s impossible to keep up. Technology is changing so fast.”
“Can we afford this?”
If you’ve noticed that you’re hearing more statements like these recently, you’re not imagining it. The telehealth train has entered the station: Systems continue to emerge in various forms, ranging from online “eye tests” to systems that offer comprehensive eye exams via remote connection are now available, all with a common goal: expanding access to services by creating new conveniences for patients. These new tools have already begun changing how patients think about eyecare, while over in the ECP’s office, technology is bringing about shifts in care delivery and coordination.
Telehealth’s recent emergence in eyecare is part of a growing movement within the broader health care arena that is reshaping the way doctors and patients interact and expanding access to care. Ocular telehealth appeals to practitioners and consumers alike for the same reasons telehealth is gaining popularity in other fields of medicine: increased access for care, greater convenience and flexibility for both staff and patient, and the potential for cost savings.
Yet legal battles over patents, regulatory issues, insurance reimbursement and ECPs’ concerns about the evolution of their role within this quickly-changing landscape—especially as messaging about the convenience of online eye tests seems to eclipse the importance of eye health—are complicating the picture. The fact that most consumers don’t understand the difference between an “eye test” and an “eye exam,” and the lack of clarity about these terms on the part of some telehealth companies is a point of contention for many eyecare practitioners.
No one has all the answers. But as you prepare to evaluate and potentially select and incorporate telehealth into your practice, you can start by asking informed questions.
OVERVIEW OF OCULAR TELEHEALTH
Examples of diagnostic procedures and images that can be captured digitally and transmitted electronically for consultation purposes include:
- Corneal topography and aberrometry
- Anterior and posterior segment imaging
- Visual fields (perimetry)
- Automated refractive technologies
- Electrodiagnostic testing
Virtual OD: Participates via live video conference, assisted by a technician who is physically present with the patient.
Mobile visual acuity testing: This category ranges from online eye tests where consumers use their digital devices to perform visual acuity tests; camera-based autorefraction. This can yield a prescription for glasses and/or contact lenses (which are often filled via the same online vendor who provides the test).
WHY TELEHEALTH? OBJECTIVES FOR YOUR PRACTICE
A key question to ask when starting out is the same one you should always ask when considering a change to procedure and investment of time and money: What efficiency and/or growth objectives do you seek for your practice, and how might this new model help achieve that? Some examples:
- Lower costs.
- Increase access to eyecare.
- Alleviate doctor shortages.
- Enhance care by being able to co-manage/ diagnose/treat in closer to real time.
- Receive enhanced training via virtual access to doctors’ demonstrations.
THE ECP’S MOTIVATION TO IMPLEMENT TELEHEALTH
Proponents of telehealth cite increased efficiency, decreased fixed costs (e.g., doctor day rates) and flexibility of scheduling as factors that will reduce the overall cost of a comprehensive exam and allow for greater exam volume resulting, in theory, in greater profits for the ECP. Some proponents also include superior access, equivalent standards of care and lowered costs among telehealth’s benefits.
Paying only for completed telehealth exams may be more economical than paying a doctor a daily rate to perform a limited number of exams each day, if there are no guaranteed minimums. In addition, real-time communication capabilities of telehealth systems are thought to further expand access to continuing education and training among practitioners. This, of course, will be impacted significantly by both insurance coverage for and reimbursement for these exams, especially in practices with fewer private-pay patients. Reimbursement varies greatly across plans and states. The official Medicaid site states: “Reimbursement for Medicaid covered services, including those with telemedicine applications, must satisfy federal requirements of efficiency, economy and quality of care. States are encouraged to use the flexibility inherent in federal law to create innovative payment methodologies for services that incorporate telemedicine technology.” Medicare Part B (Medical Insurance) covers “certain services, like office visits and consultations, that are provided: using an interactive two-way telecommunications system (with real-time audio and video); and by a doctor or certain other health care provider who isn’t at your location.”
USERS’ MOTIVATION TO IMPLEMENT THESE PRACTICES
Many opine that overall, telehealth will facilitate greater access to quality services and in turn expand public health awareness. If telehealth also results in lower exam costs for patients and is covered by insurance plans, we should also see an increase in the frequency with which they seek care.
Telehealth is often extolled as a way to expand access to care for rural and otherwise underserved populations, and for homebound patients in any setting, telehealth can transcend transportation limitations. In some cases, remote care can also ameliorate fear of doctors and/or clinical settings, germs, etc.
Telehealth is also the logical extension of our increasingly tech-dependent consumer mindset, offering greater convenience for busy patients even if they reside in practice-rich areas, as well as enhanced diagnostics and care coordination among collaborating providers and specialist. As 20/20 contributing editor Barry Santini notes, “The doctor is out, the consumer is in. Tech is freeing the consumer from being a passive participant in eyecare— patients are now starting to drive the experience.” Additionally, telehealth is not only appealing to younger patients such as tech-dependent Millennials: Older patients are inclined to accept and engage with remote and digital practices nearly as much as their younger counterparts.
ADDITIONAL CONSIDERATIONS
Necessary personnel, and their roles and responsibilities: What will the evolved doctor-patient relationship look like? What are the other staff member roles? Telehealth requires a collaborative approach, often interdisciplinary, almost always expanding the involvement of third parties external to your practice.
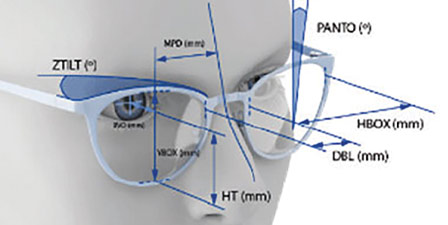
Tools: System requirements for real-time communication, store-and-forward and remote patient monitoring include reliable internet service, with ample speed and enough bandwidth to accommodate all of the above. This is vital to the entire process, especially live video conferencing that allows participants to interact in real time.
Training: It’s essential to train your staff on instrumentation and communication tools properly, including production of ocular imagery plus: operation of video conferencing, data storage and management, and coordination of care if applicable.
Trial runs: Offices using the virtual and collaborating OD models will require updated procedures and protocol, so before launch, staff should test the setup to ensure proper flow, functionality, accuracy, et al., in a controlled environment.
Costs: Depending on which type of telehealth you implement, costs can vary widely depending on the tools (including equipment), in addition to IT-related systems, plus training. It may make sense to hire a consultant to do the legwork of research and implementation. Insurance coverage and reimbursement for telehealth varies greatly across services and states, though we’ll likely see greater adoption if it proves to lower the cost of services in the long run while maintaining or enhancing quality of care.
Commitment to best practices: How do we evaluate all of this, knowing full well that regulation and legislation are not occurring as fast as technological development? Another pertinent note from Barry Santini: “Standards of care are going to end up being redefined by technology.” ECPs planning to incorporate telehealth into their practices, as well as those who are post-implementation, need to stay on top of changing definitions and standards of care in this rapidly-evolving landscape.
TO BE OR NOT TO BE
As the saying goes: Be at the table, not on the menu. Times are changing—and fast. The ECP’s first and foremost priority should be to deliver the highest-quality patient care, without compromising outcomes. A virtual OD visit that does not simulate examination conditions that adhere to established best practices may well result in problems ranging from Rx re-dos to missed or inaccurate diagnoses. Certainly, the advances in technology which enhance ocular imagery, improve coordination of care by speeding the exchange of accurate information between provider and patient, and expand access to quality eyecare for those in rural or underserved areas will be a boon to eyecare service delivery—but are those benefits enough to warrant the potential risks involved before a solid clinical evidence base is established? Additional regulatory considerations include how to ensure licensure/credentialing of all parties partaking in the process and of course, data privacy.
For those who have just begun wading through the growing complicated body of information regarding telehealth and asking themselves how they should begin to navigate this, a simple rule of thumb is: Be Aware, Be Involved, Be Transparent and Be Proactive. Read up on the latest developments in this subsector, attend webinars and conferences dedicated to new technologies and the regulatory issues surrounding them, and communicate with as many stakeholders as possible: your ECP peers, vendors, regulatory bodies involved in evaluating standards of care; and don’t forget your patients.
If and when you decide to begin incorporating teleoptometry procedures, prepare patients for the modifications to the “old exam” they expect. In the “virtual OD” model, many patients will question, or even respond poorly to, the absence of a doctor, possibly presuming that it’s a cost-cutting measure that will compromise the care and attention they are receiving. Assuaging these concerns will be a crucial aspect of integrating new tools and methods into your practice, so preparation and open communication will be essential.
Due to the limitations of “vision test” mobile apps which enable users to renew spectacle and contact lens prescriptions but currently do not/cannot properly evaluate eye health (and the current regulatory climate), we’re likely still quite a ways from “replacing the eye doctor with a smartphone,” but for now, ECPs would be well served to assess how well they are communicating the value of each step of the comprehensive eye exam to their patients. A frequent criticism of online eye tests is that they misrepresent what’s being performed, either by not explicitly stating that they are not in fact comprehensive exams, and/or not sufficiently promoting the necessity of doctor visits to examine eye health hand-in-hand with vision testing. Any practice using teleoptometry should steer clear of these pitfalls and commit to providing clear, transparent information to patients with regards to use of telehealth processes.
The appeal of telehealth is not only in its potential to expand eyecare provision and build up one’s practice; it is also promising for ODs who seek greater flexibility, including those with families, are homebound, or have physical limitations or disabilities. Ocular telehealth also offers ample opportunities for training and demonstration across geographic borders and thus the potential to enhance quality of care, especially in areas that have a doctor shortage or other limitations. Whether you’re just starting to think about which telehealth system(s) make sense for your practice, or you’re post-implementation, technology-fueled change—with its ever-accelerating pace—is upon us; these are uncertain times, but with the potential these new models hold, they can also be exciting times. Take a deep breath and dive in.
Who’s Who in Ocular Telehealth
The following companies are among a growing number that offer ocular telehealth products and services. Here’s how they describe themselves, in their own words.
20/20NOW systems leverage “state-of-the-art technology, digital equipment, high-definition audio/video, certified optical technicians and licensed doctors [to] perform a thorough and comprehensive exam [which] includes both objective and subjective testing, extensive screening for eye problems and diseases such as glaucoma, macular degeneration and diabetic retinopathy, as well as screening for systemic health diseases like diabetes and hypertension.”
ADAPTICA, based in Italy, is a “mobile, wireless refraction system [which] offers diversified solutions in all those areas in which images generated by optical systems need to gain focus, sharpness and optical quality,” including the 2WIN, “a binocular refractometer for the most reliable subjective and objective examination.”
DIGITALOPTOMETRICS allows “patients at an optical exam location to receive a ‘comprehensive eye health examination’ performed by a licensed optometrist from a location remote from the patient,” using “live remote video conference between the optometrist and patient and remote operation of optical equipment.”
ESSILOR’s website provides seven online tests “to help you quickly and easily know if it’s time to have a more detailed eye examination with a vision care professional.”
EYENETRA offers a “self-test mobile [auto]refraction tool powered by a smartphone for mobile eye diagnostics or vision screenings” via “a series of game-like interactions in a virtual-reality environment,” as well as an automated lensometer and a handheld phoropter.
EYEQUE is “dedicated to… putting affordable, accurate, self-administered vision tests directly into [peoples’] hands around the world, to test and track vision changes over time, instantly access results in-app and online, and conveniently share data with doctors.”
GLOBECHEK is a “teleophthalmology” service that offers consumers “convenient, affordable access to comprehensive eye screening.” Screenings are performed by a globe-shaped kiosk that houses diagnostic instruments. Test results are interpreted by a GlobeChek certified ophthalmologist.
OPTERNATIVE’s “anywhere, anytime” 15-minute online test is presented to consumers as “all you need to get a renewed prescription for contacts or glasses within 24 hours… for use wherever you buy contacts or glasses. Your personalized vision test will measure how you see, but won’t check the health of your eyes… a prior prescription is required most of the time.”
PEEK SOLUTIONS is a social enterprise “built on smartphone technology, [which] includes apps and hardware enabling eye checks to be conducted in homes, communities and schools. This generates data which ensures patients are linked to appropriate treatment and resources are allocated efficiently.”
PLENOPTIKA, another social enterprise spun out of the Massachusetts Institute of Technology, was formed “to respond to the problem of low vision suffered by more than a billion people worldwide. QuickSee by PlenOptika enables accurate autorefraction anywhere, at the touch of a button,” and has been tested “across both low and high resource settings.”
SIMPLE CONTACTS promotes “[contact] lenses you need, doctor visits you don’t: renew your contact lens prescription with our doctor-designed vision test and reorder your lenses—from anywhere, on your schedule.”
SMART VISION LABS' mission is to “increase access to vision care by leveraging innovation and technology.” The company encourages ECPs to “grow [their] business with optical telemedicine” by offering “vision exams during all business hours without appointments” via a “convenient, affordable, clinically proven 5-Minute Vision Test and proprietary telemedicine platform” which “reduces costs and improves sales and ROI for our partners.”
WARBY PARKER’s Prescription Check “is a telehealth service that allows an eye doctor to assess how [users] are seeing through [their] glasses and provide an updated glasses prescription [currently only for those wearing a distance-only Rx].”
ZEISS offers a “Visual Acuity Check, Contrast Vision Check, & Colour Vision Check” on its website, to help users “quickly and easily determine whether it’s time to have a professional eyesight test.”
Also of interest: While not “telehealth” per se, GLASSESUSA.COM offers an online prescription scanner application that extracts the “optical parameters” off the wearer’s current pair so they can order new glasses online.
The AOA’s Point of View
At the 2018 Vision Monday Global Leadership Summit, several prominent industry figures lent their voices to panels on the subject. Michael Duenas, OD, chief public health officer of the American Optometric Association, stated that the organization’s first and foremost focus “is to uphold and advance evidence-based standards of care that ensure patient health and safety. To that end, the AOA embraces telehealth and advanced technologies with ocular telehealth fitting into the matrix of patient care when it furthers patient health. To accomplish these goals, telehealth technologies must: 1. Be responsible-science and evidenced based, 2. Embrace patient health, and 3. Support the patient-doctor relationship.”
For more information about the AOA’s view of telehealth, see the “Position Statement Regarding Eye and Vision Telehealth Services” posted on www.aoa.org.
Contributing editor Sara Bonizio is marketing & community relations manager for Metro Optics Eyewear in Bronx, N.Y.